IASLC Neoadjuvant Therapy in Lung Cancers Initiatives
Overall Goal: To establish pathologic response in surgical resection specimens following neoadjuvant therapies as predictors of long-term clinical benefit in patients with stages II to III lung cancers.
The IASLC is working to address key knowledge gaps in clinical practice related to the use of neoadjuvant therapies in lung cancer through the establishment of the IASLC Neoadjuvant Therapy in Lung Cancers Initiative. These projects aim to knowledge gaps by providing clear definitions and guidance for the lung cancer community to rely on , with the ultimate goal of establishing pathologic response in surgical resection specimens following neoadjuvant therapies (MPR and pCR) as predictors of long-term clinical benefit in patients with stages I to III lung cancers.
Phase 0: Organize, Host, and Report Consensus Opinions from the FDA-IASLC Workshop on Neoadjuvant Therapy in Lung Cancers.
Phase 1: Publish IASLC recommendations to process and analyze resection specimens after neoadjuvant therapy and report results of pathologic response.
In order to address the lack of uniform processing and response definitions, the IASLC published an article in the Journal of Thoracic Oncology outlining detailed recommendations on how to process lung cancer resection specimens and to define pathologic response including major pathologic response and complete pathologic response following neoadjuvant therapy. A standardized approach is recommended to assess the percentage of 1) viable tumor, 2) necrosis, and 3) stroma (including inflammation and fibrosis). These recommendations are intended as guidance for clinical trials, although it is hoped they can be viewed as a suggestion for good clinical practice outside of clinical trials to improve the consistency of pathologic assessment of treatment response.
Phase 2: IASLC Reproducibility Study
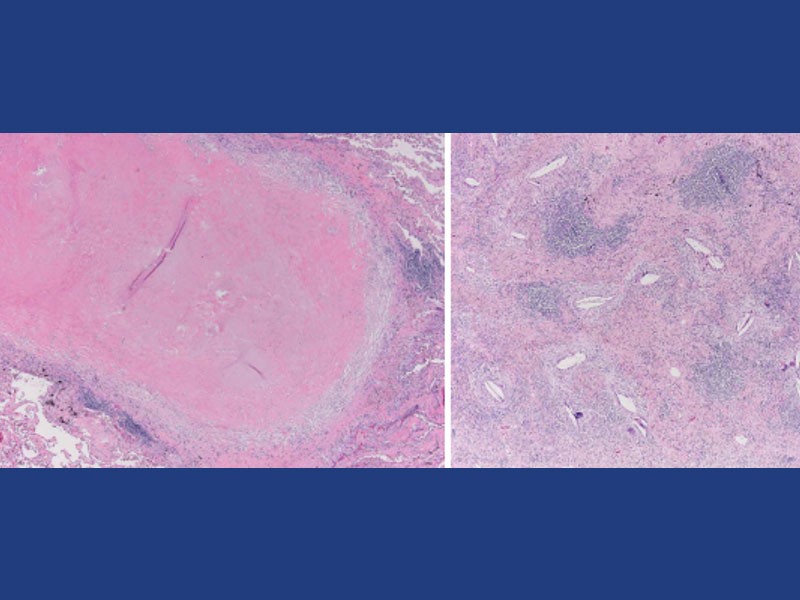
The IASLC Reproducibility Study aims to determine reproducibility among pathologists of pathologic response determinations using the IASLC multidisciplinary recommendations for pathologic assessment of lung cancer resection specimens following neoadjuvant therapy. This study brings together an international cohort of 11 pathologists to evaluate 60-90 NSCLC tumors, including both adenocarcinoma and squamous cell carcinomas histologies, that received anti-PD-1 or PD-L1 alone or in combination with chemotherapy or anti-CTLA-4 therapy, treated in a clinical trial to ensure proper sampling of the resected specimen. This initiative is currently ongoing but is expected to conclude with a publication in the Journal of Thoracic Oncology in mid-2023.
Phase 2B: IASLC Digital Quantification of Pathologic Response in Neoadjuvant Treated Non-Small Cell Lung Cancer (NSCLC)

In this project, PathAI and IASLC will collaborate to apply an AI-driven digital pathology assessment of pathologic response and compare this to manual assessments from the 11 pathologists participating in the IASLC Pathologic Response Interobserver study. PathAI will use neoadjuvant lung cancer quantification algorithms on the 60-90 NSCLC tumors from clinical trials using immune checkpoint inhibitors. These algorithms will allow us to classify cases by the level of pathologic response achieved through digital quantification of the percent viable tumor remaining after neoadjuvant therapy. The use of AI to determine pathologic response presents advantages such as high-resolution, fully quantitative assessments and a high level of standardization and reproducibility. This study will support the validation of an AI-powered assessment of pathological response, which could potentially be used as a clinical endpoint in studies of neoadjuvant treatment to predict survival benefits at the time of surgery.
Phase 3: Lung Cancer Neoadjuvant Trial Endpoint Database (LCNTED)
In the final phase of the IASLC Neoadjuvant Therapies in Lung Cancer Initiative, aims to accomplish the ultimate goal of establishing pathologic response in surgical resection specimens following neoadjuvant therapies (MPR and pCR) as predictors of long-term clinical benefit in patients with stages I to III lung cancers. This process has been accomplished in the CTNeoBC pooled analysis project analyzing neoadjuvant trials in breast cancers.
Following the lead of CTNeoBC in breast cancers, Phase 3 of the initiative will:
- Establish the association between pathologic response and event-free survival (EFS) and overall survival (OS)
- Establish the definition of pathologic response, including MPR and CPR that correlates best with long-term outcomes
- Identify the lung cancer subtypes in which pathologic response best correlate with long-term outcomes
- Assess whether increases in pathologic response between treatment groups predict improved EFS and OS
An initiative of this magnitude and importance requires the collaboration of many partners and stakeholders, as no one organization or company can act alone to make meaningful progress. Therefore, this initiative will bring together the IASLC membership, FDA regulators, and various leading industry partners, who all share the common goal of eliminating lung cancer as a cause of death.